Welcome to The House Institute
Our History
The House Institute is the preeminent center for the treatment of ear disease and neurological disorders. For more than 60 years, the House Institute’s neurotologists and neurosurgeons have led the way in treating the causes of hearing, balance and skull-base disorders with cutting-edge practices and procedures.
The Los Angeles-based team’s audiological staff works in close conjunction with its physicians to provide the most advanced audiometric evaluations and treatment options to ensure that patients receive the best treatment possible.
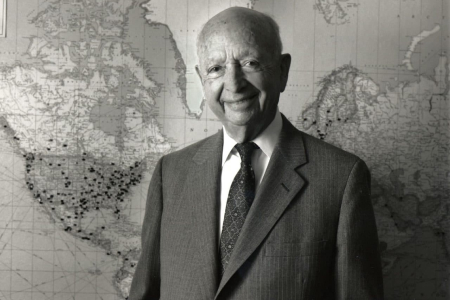
Named for the groundbreaking work done by founder Howard P. House, M.D., the House Institute treats a variety of ear-related disorders, including Meniere’s disease, acoustic neuromas, skull-base tumors, neurofibromatosis, surfer’s ear, balance issues, chronic ear infections and much more.
Serving the communities of greater Los Angeles and Orange County with both clinical locations and hearing aid dispensaries, the House Institute also includes a 501-(c)(3) private nonprofit branch, the House Institute Foundation (formerly House Ear Institute), that has pioneered innovative research in otology, neurotology and neurosurgery.
World Class Care, With First Class Service


The House Institute Hearing Health Centers
We provide hearing healthcare solutions and hearing aid service suited for your individual needs with Hearing Health Centers located in Bakersfield, Encino, Santa Monica, Orange County and downtown Los Angeles.

The House Institute Foundation
The House Institute Foundation (HIF) is a leading hearing health nonprofit focusing on neuroscience and ear research, education, and global hearing health. For over 75 years, HIF has been making groundbreaking discoveries in hearing science, providing professional and public health education programs, and increasing access to treatments, technology, and training in high-need communities locally and worldwide.

House Clinic
House Clinic consists of an elite team of audiologists, otolaryngologists, neurotologists and neurosurgeons who are leaders in treating the causes of hearing, balance and skull-base issues and other complex neurosurgical disorders with advanced practices and procedures. The team treats a variety of ear-related disorders such as Meniere’s disease, acoustic neuromas, skull-base tumors, neurofibromatosis, and other complex neurological and neurosurgical disorders.

The House Institute Children’s Center
The House Children’s Hearing Center is a comprehensive hearing center devoted to the evaluation, diagnosis, and treatment of the full spectrum of hearing conditions in children, from birth to 18 years of age. Our primary goal is to ensure every child that comes through our doors receives the world-class care our 75-year history of ear and neuroscience expertise can provide.